You’re sitting quietly in your favorite chair, maybe reading a book or watching TV, when it happens, your heart suddenly starts hammering in your chest like you’ve just run a marathon. But you haven’t moved. You haven’t been scared. You’re just… sitting there. And now your mind races faster than your heart: Is something wrong with me? Should I call someone? Am I having a heart attack?
Take a breath. You’re not alone in this moment of panic, and chances are, you’re going to be just fine.
This sensation, that unexpected flutter, pound, or race in your chest, is what doctors call heart palpitations. It’s one of the most common concerns people bring to their healthcare providers, affecting up to 16% of patients during primary care visits. What’s interesting is that women experience them more frequently than men, often linked to the hormonal roller coaster of menstrual cycles, pregnancy, and menopause.
Here’s what most people find reassuring: the vast majority of palpitations are completely harmless. Your heart isn’t broken; it’s just having a moment. That said, sometimes that racing heart is trying to tell you something worth listening to.
In this guide, we’re going to walk through everything you need to know about unexplained fast heartbeats. We’ll explore the science behind what’s happening in your chest, the surprising everyday triggers that might be causing it, the warning signs that mean you should see a doctor, how medical professionals diagnose the issue, and practical steps you can take right now to calm things down. All of this is backed by research from trusted sources like the Mayo Clinic, Cleveland Clinic, and the American Heart Association.
By the time you finish reading, you’ll have the knowledge to approach this with confidence instead of fear. Let’s dive in.
What’s Really Happening in There with Racing Heart?
To understand why your heart sometimes feels like it’s auditioning for a drum solo, let’s talk about how this incredible organ actually works.
Your heart is essentially a sophisticated pump powered by its own electrical system. Picture the wiring in your house, when everything’s working properly, the lights come on smoothly, appliances hum along, and you don’t think twice about it. But when there’s a surge or a flicker, suddenly you notice.
Under normal, calm conditions, your heart beats between 60 and 100 times per minute. That’s your resting heart rate, the steady rhythm that keeps blood flowing to every corner of your body without you having to think about it. Each beat starts with an electrical impulse from your heart’s natural pacemaker, called the sinoatrial (SA) node, located in the upper right chamber. This signal travels through specialized pathways to coordinate the squeezing and relaxing of all four chambers in perfect harmony.
But sometimes, this electrical system hits a snag. When your heart beats faster than 100 times per minute, doctors call it tachycardia. When you feel those beats, whether they’re fast, fluttering, pounding, or skipping, those are palpitations.
There are different types of rapid heartbeats, and understanding the distinction matters:
Sinus tachycardia is when your heart speeds up normally but maintains its regular rhythm. This is what happens when you’re exercising, nervous before a presentation, or startled by a loud noise. Your body is responding appropriately to a demand, it’s just that sometimes the demand is emotional rather than physical.
Supraventricular tachycardia (SVT) is when faulty electrical signals from above the heart’s lower chambers (ventricles) cause sudden bursts of rapid beating. It affects about 2 in 1,000 people and can make your heart race to 150-250 beats per minute in an instant, often feeling like it starts and stops abruptly, like someone flipped a switch.
Atrial fibrillation (AFib) is an irregular, often rapid heart rhythm where the upper chambers quiver chaotically instead of beating effectively. Recent estimates suggest it affects over 10 million U.S. adults, three times what we thought just two decades ago, thanks to better detection methods. This one’s worth paying attention to because it can increase stroke risk if left untreated.
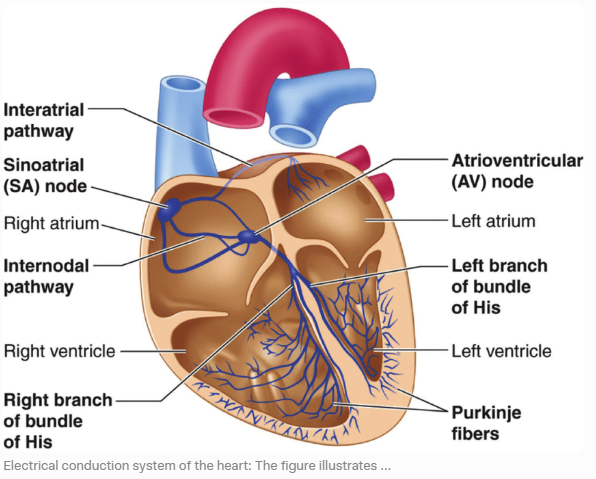
Think of your heart’s electrical system like an orchestra. Usually, the conductor (your SA node) keeps everyone in perfect time. But sometimes a musician jumps in too early, or a whole section suddenly speeds up, and you get that chaotic, unsettling feeling in your chest. Sometimes it’s a brief disruption that corrects itself. Other times, it needs some help getting back on track.
Here’s something fascinating that emerging research has revealed: your brain and heart are in constant conversation. The field of neurocardiology shows that palpitations aren’t just about the heart, they involve complex brain-heart connections and even how aware you are of your own body’s internal sensations (something called cardioception).
Factors like stress, body composition, and psychological state all influence this awareness. This is why two people with identical heart rates might have completely different experiences, one might not notice anything unusual, while the other feels every single beat.
The good news? Most palpitations are what we call “benign”, they come and go without causing any harm or indicating serious disease. But understanding what’s happening gives you the power to identify when it’s just a false alarm versus when your heart is genuinely signaling for help.
Common Causes: The Everyday Triggers You Might Not Expect
Here’s where things get interesting. When people say their heart is racing “for no reason,” there’s almost always a reason, it’s just not always obvious.
A comprehensive study found that when doctors investigate palpitations, they discover cardiac (heart-related) causes in 43% of cases, psychiatric causes in 31%, miscellaneous triggers like medications or caffeine in 10%, and genuinely unknown causes in only 16%.
That means in most cases, we can figure out what’s going on. Sometimes it’s as simple as connecting the dots you didn’t know were there.
Lifestyle and Environmental Elements
Stress and Anxiety
This is one of the main reasons palpitations occur, accounting for 30-40% of cases. When you’re stressed, anxious, or panicking, your body activates its “fight or flight” response, a survival mechanism that’s been with us since we were running from predators. Your brain releases adrenaline and cortisol, hormones that prime you for action by increasing your heart rate and blood pressure.
The tricky part? You don’t need to be facing a life-threatening situation for this to kick in. Your body can’t tell the difference between a tiger chasing you and a looming work deadline, an argument with a loved one, or scrolling through anxiety-inducing news. Given that anxiety disorders affect about 19% of adults each year, it’s no wonder so many people experience stress-related palpitations.
Panic attacks can be particularly convincing mimics of heart problems. The chest tightness, racing heart, shortness of breath, and sense of impending doom feel so physical that many people experiencing their first panic attack end up in the emergency room, certain they’re having a heart attack.
Caffeine, Alcohol, and Other Stimulants
That morning coffee, afternoon energy drink, or evening glass of wine might be more involved than you think. Caffeine is a stimulant, that’s why we love it, but it directly stimulates your nervous system and can increase your heart rate. Even moderate amounts can trigger palpitations in sensitive individuals.
Alcohol creates a different problem. It dehydrates you, which thickens your blood and makes your heart work harder. It can also irritate heart tissue and disrupt normal electrical signals, particularly if you drink heavily or binge drink. There’s even a term for it: “holiday heart syndrome,” coined after doctors noticed people showing up with irregular heartbeats after weekends or holidays involving heavy drinking.
Don’t forget about hidden stimulants: nicotine from cigarettes or vaping, pseudoephedrine in over-the-counter cold medications, diet pills, some asthma inhalers, and yes, even recreational drugs like cocaine or methamphetamine, which are particularly dangerous for your heart.
One pattern I’ve observed: people rarely connect their third or fourth cup of coffee with palpitations that happen an hour later. Start tracking your caffeine intake and timing, you might spot a pattern that surprises you.
Hormonal Changes
Hormones are powerful chemical messengers, and when they shift, your heart feels it. This is why palpitations are more common in women and often cluster around specific times:
- Menstrual cycles: Estrogen and progesterone levels fluctuate throughout the month, and some women notice palpitations right before or during their period.
- Pregnancy: Blood volume increases by up to 50% during pregnancy, and your heart rate naturally increases to pump all that extra blood. Add hormonal surges, and palpitations become extremely common.
- Menopause: The dramatic decrease in estrogen can trigger palpitations, often accompanied by hot flashes and night sweats.
- Thyroid disorders: Hyperthyroidism (overactive thyroid) affects 1-2% of adults and speeds up your entire metabolism, including your heart. People with hyperthyroidism often feel like they’re running on fast-forward: racing heart, weight loss despite eating normally, feeling constantly warm, and experiencing anxiety or tremors.
Dehydration, Diet, and Exercise:
Your heart is a muscle that relies on proper fluid balance and nutrients to function optimally. When you’re dehydrated, your blood volume decreases and becomes more concentrated, forcing your heart to beat faster to circulate it effectively. This is why you might notice palpitations after a sweaty workout if you haven’t been drinking enough water, or at the end of a long day when you’ve been too busy to hydrate.
Blood sugar swings matter too. Skip breakfast, and by mid-morning your blood sugar might drop, triggering a stress response that includes a faster heartbeat. Eating a massive meal, especially one high in carbohydrates or very spicy foods, can sometimes trigger palpitations as blood rushes to your digestive system.
As for exercise, intense workouts naturally elevate your heart rate, that’s the point. But sometimes the palpitations come afterward, during recovery, particularly if you’ve pushed yourself hard without proper conditioning or if you’re dehydrated.
Medications and Substances
More medications can affect your heart rate than you might realize. Asthma inhalers (particularly albuterol), certain antibiotics, antidepressants, thyroid replacement hormones if the dose is too high, ADHD medications, and even some supplements can trigger palpitations.
Interestingly, stopping certain medications can also cause problems. If you’ve been taking beta-blockers (a type of blood pressure medication that slows the heart) and suddenly stop, you might experience rebound tachycardia.
Even supplements aren’t always innocent. High doses of omega-3 fatty acids, certain herbal supplements, or excessive vitamin D can occasionally trigger heart rhythm changes.
Medical Conditions Lurking Beneath the Surface
Sometimes the cause runs deeper than lifestyle factors. These conditions might be silently contributing to your racing heart:
Anemia: When you don’t have enough healthy red blood cells to carry oxygen to your tissues, your heart compensates by pumping faster. This is why people with anemia often feel their heart racing with minimal exertion, climbing a single flight of stairs might leave them breathless and pounding.
Electrolyte imbalances: Your heart’s electrical system depends on precise levels of potassium, magnesium, calcium, and sodium. Taking diuretics (water pills), excessive sweating, vomiting, or diarrhea can throw these off balance. Low potassium is a particularly common culprit.
Fever and infections: When your body is fighting an infection, your metabolic rate increases, and so does your heart rate, typically about 10 beats per minute for every degree Fahrenheit your temperature rises.
Heart-specific conditions: This category includes actual cardiac arrhythmias (AFib, SVT, premature ventricular contractions), structural issues (mitral valve prolapse, where a heart valve doesn’t close properly), cardiomyopathy (disease of the heart muscle itself), or congenital problems you might have been born with.
Rare but important conditions include Wolff-Parkinson-White syndrome, where an extra electrical pathway in the heart can cause sudden rapid heartbeats, and hypertrophic obstructive cardiomyopathy (HOCM), a genetic condition where the heart muscle is abnormally thick. These are uncommon, but they’re worth ruling out, especially if you have a family history of sudden cardiac death or if palpitations occur during exercise.
Postural Orthostatic Tachycardia Syndrome (POTS): This condition causes your heart rate to increase dramatically when you stand up, often by 30 beats per minute or more within 10 minutes of standing. It primarily affects young women and can cause dizziness, lightheadedness, and palpitations. It’s often misdiagnosed as anxiety.
Comparing Benign vs. Concerning Causes
Here’s a more comprehensive comparison to help you categorize what you’re experiencing:
| Benign Causes | Typical Pattern | Concerning Causes | Typical Pattern |
| Stress/Anxiety | Brief episodes tied to identifiable worry or panic; stops when you calm down | AFib/SVT | Irregular rhythm that lasts minutes to hours; may feel chaotic rather than just fast |
| Caffeine/Alcohol | Occurs within 30-60 minutes of consumption; resolves within hours | Hyperthyroidism | Persistent elevated heart rate with weight loss, heat intolerance, constant fatigue |
| Dehydration | Accompanied by thirst, dark urine, dry mouth; improves with hydration | Anemia | Chronic tiredness, pale skin, shortness of breath with minimal activity, cold hands/feet |
| Hormonal Shifts | Tied to menstrual cycle, pregnancy, or menopause; cyclical pattern | Cardiomyopathy | Family history of heart disease, swelling in legs/ankles, exercise intolerance, chest discomfort |
| Fever/Fatigue | Only during illness; heart rate returns to normal when fever breaks | Valve Problems | Heart murmur detected by doctor, chest pain, fainting spells, progressive shortness of breath |
| Post-exercise | During or immediately after vigorous activity; gradually normalizes with rest | POTS | Dramatic increase upon standing, accompanied by dizziness, brain fog, near-fainting |
The key to distinguishing between these is pattern recognition. Start keeping a log, even just notes on your phone, of when palpitations occur, what you were doing, what you’d consumed, your stress level, and how long they lasted. Studies show that about 40% of causes can be identified through history and physical exam alone, meaning your detailed observations are genuinely valuable diagnostic information.
Red Flags and Serious Signs You Shouldn’t Ignore
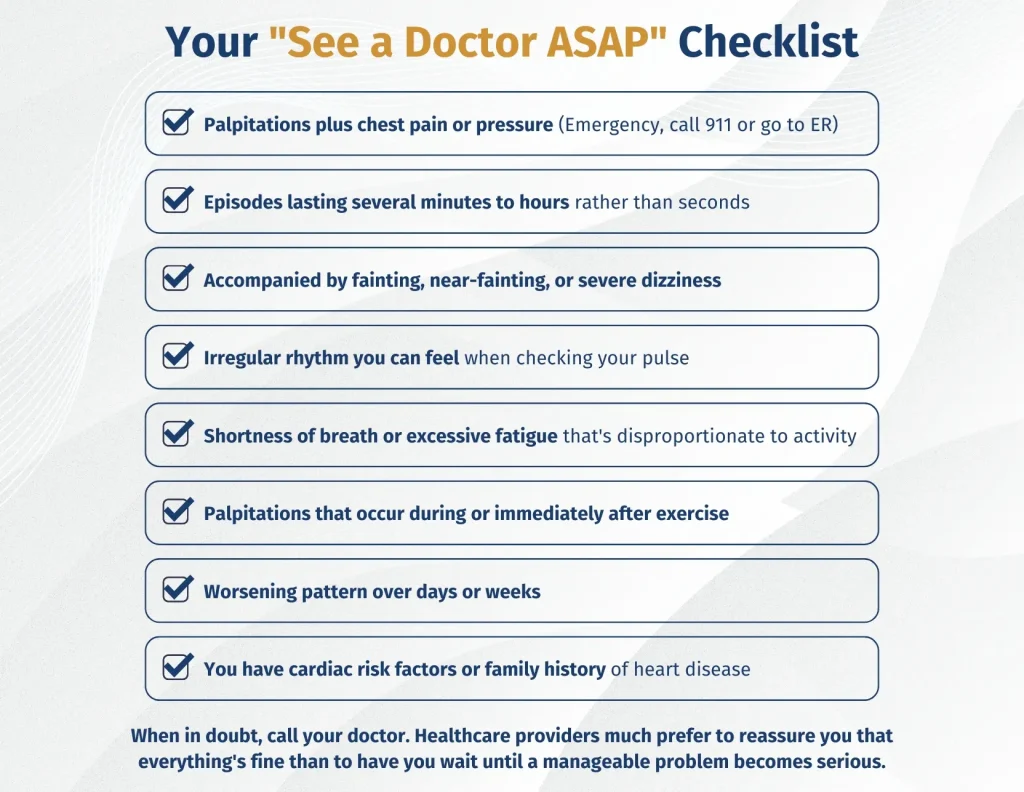
Most palpitations are like a car’s “check engine” light coming on briefly and then turning off, a momentary glitch that doesn’t indicate a serious problem. But some warning signs mean it’s time to take your car (or in this case, your heart) to the mechanic right away.
Here’s the essential question: When does a racing heart cross the line from “annoying but harmless” to “potential medical emergency”?
The Red Flags That Mean “See a Doctor Now”
Chest Pain or Pressure: This is non-negotiable. If your racing heart comes with chest pain, pressure, tightness, or a squeezing sensation, especially if it radiates to your jaw, neck, shoulder, or arm, you need emergency care immediately. This could indicate angina, a heart attack, or a serious arrhythmia. Don’t convince yourself it’s just heartburn or anxiety. Better to be checked and reassured than to wait and risk serious damage.
Dizziness, Fainting, or Near-Fainting: If your racing heart makes you feel dizzy, lightheaded, or like you might pass out, it means your heart isn’t pumping blood effectively to your brain. This is dangerous for two reasons: you could fall and injure yourself, and it might indicate a serious rhythm problem. Actual fainting during palpitations is especially concerning and warrants immediate evaluation.
Shortness of Breath: Feeling like you can’t catch your breath or needing to gasp for air while your heart is racing, particularly if you’re not exerting yourself, suggests your heart and lungs aren’t working together efficiently. This can indicate heart failure, significant arrhythmia, or pulmonary issues.
Persistent Rapid or Irregular Heartbeat: If your heart rate stays above 110-120 beats per minute while you’re resting, or if you can feel an irregular, chaotic rhythm (versus just fast), this could be atrial fibrillation or another arrhythmia. AFib particularly concerns doctors because it allows blood to pool in the heart chambers, potentially forming clots that can cause stroke.
Palpitations During Sleep or Upon Waking: Waking up with your heart pounding, or being jolted awake by a racing heart, isn’t normal. Your heart rate should be at its lowest during sleep. Nocturnal palpitations can indicate sleep apnea, heart rhythm disorders, or other issues that deserve investigation.
Palpitations During or Triggered by Exercise: While it’s normal for your heart to beat faster during exercise, palpitations that feel abnormal, irregular, or excessive during activity, especially if accompanied by chest discomfort or extreme fatigue, could indicate exercise-induced arrhythmias or underlying heart disease.
You Have Risk Factors: Your personal health context matters enormously. Palpitations deserve more serious attention if you:
- Are over 50 years old (risk of heart disease increases with age)
- Smoke or have smoked
- Have high blood pressure, high cholesterol, or diabetes
- Are significantly overweight or obese
- Have a family history of heart disease, especially sudden cardiac death in young relatives
- Have existing heart disease or have had a previous heart attack
Additional Warning Signs Worth Noting
Progressive worsening: Palpitations that are becoming more frequent, lasting longer, or feeling more intense over time shouldn’t be ignored.
Very slow heart rate: A resting heart rate below 45 beats per minute (unless you’re an endurance athlete) combined with dizziness might indicate a conduction problem where electrical signals aren’t traveling properly through your heart.
New irregular rhythm you can feel: If you place your fingers on your pulse at your wrist or neck and feel that beats are coming in an irregular pattern, not just fast, but unpredictably irregular, this suggests an arrhythmia rather than simple sinus tachycardia.
Injury from fainting: If you’ve actually lost consciousness and hurt yourself falling, this is an emergency situation requiring immediate evaluation.
What the Statistics Tell Us
Here’s something encouraging: in about 84% of palpitation cases, doctors successfully identify a cause. Of those causes that are identified, 43% turn out to be cardiac, 31% are psychiatric (primarily anxiety), and 10% are miscellaneous (medications, caffeine, etc.).
What this means for you: There’s an excellent chance that with appropriate evaluation, you’ll get answers. And even better, most of those answers indicate treatable or manageable conditions rather than life-threatening disease.
The diagnostic approach follows a logical sequence, starting with the simplest, least invasive tests and only proceeding to more complex testing if needed. Most people get their answers from a basic evaluation: history, physical exam, ECG, and blood tests.
Treatment and Prevention
Once you understand what’s causing your palpitations, the path forward becomes much clearer. Treatment is highly individualized, but for the vast majority of people, it starts with lifestyle modifications before ever considering medications or procedures.
Lifestyle Modifications
These changes sound simple, but they’re genuinely powerful. Research shows that lifestyle interventions can reduce or eliminate palpitations in a significant percentage of cases where they’re benign.
Caffeine and Alcohol
You don’t necessarily have to quit entirely (unless your doctor advises it), but strategic reduction often works wonders. Try limiting caffeine to under 200mg daily, that’s roughly two 8-ounce cups of coffee. Switch to decaf for your third cup, or replace afternoon coffee with herbal tea.
For alcohol, the key is moderation and consistency. Binge drinking (consuming 4-5 drinks within two hours) is particularly hard on your heart’s electrical system. If you drink, spread it out and stay hydrated, drink a glass of water between alcoholic beverages.
Hydration
Aim for at least eight 8-ounce glasses of water daily, more if you’re exercising or it’s hot outside. A good rule of thumb: if your urine is darker than pale yellow, you need more water. Proper hydration keeps your blood volume adequate, helps maintain electrolyte balance, and reduces the work your heart has to do.
Nutrition
Focus on potassium-rich foods (bananas, sweet potatoes, spinach, avocados, beans) and magnesium-rich foods (nuts, seeds, whole grains, dark leafy greens, dark chocolate). These minerals are essential for proper cardiac electrical function.
Eat regular, balanced meals to avoid blood sugar swings. If you’re prone to palpitations, pay attention to whether very large meals or specific foods trigger episodes, some people find that high-carb or very spicy meals are culprits.
Exercise
Regular exercise actually stabilizes heart rhythm over time. Aim for at least 150 minutes of moderate activity weekly, brisk walking, swimming, cycling. The key is gradual progression. Don’t go from sedentary to running marathons. Build up slowly.
If you experience palpitations during exercise, that’s worth discussing with your doctor before continuing intense activity. But for most people, consistent moderate exercise reduces palpitations over time by improving cardiovascular fitness and reducing stress.
Maintain a Healthy Weight
Obesity stresses your heart and increases the risk of conditions like sleep apnea and AFib. Even modest weight loss, just 5-10% of body weight, can significantly improve cardiovascular health.
Sleep
Aim for 7-9 hours of quality sleep nightly. Sleep deprivation increases stress hormones, disrupts your autonomic nervous system, and can trigger palpitations. If you snore heavily or feel unrested despite adequate sleep time, talk to your doctor about screening for sleep apnea, a condition closely linked to heart rhythm problems.
Stress Management: Breaking the Cycle
This might be the most important intervention of all, given that stress and anxiety account for 30-40% of palpitations. Find what works for you:
- Mindfulness meditation: Even 10 minutes daily can reduce baseline stress and your reactivity to stressors.
- Deep breathing exercises: Simple but effective. Try the 4-7-8 technique: breathe in for 4 counts, hold for 7, exhale for 8.
- Yoga or tai chi: Combines physical activity with breath work and meditation.
- Cognitive behavioral therapy (CBT): Particularly helpful if anxiety is driving your palpitations. CBT teaches you to identify and change thought patterns that fuel anxiety.
- Regular leisure activities: Whatever brings you joy and relaxation, reading, gardening, painting, playing with pets.
Quit Smoking
If you smoke, quitting is the single most impactful thing you can do for your heart. Nicotine directly stimulates your heart and increases blood pressure. Within just weeks of quitting, your cardiovascular risk begins to drop. Ask your doctor about smoking cessation programs, success rates are much higher with support.
Download your Guide for Home Remedies Techniques Now!
When Palpitations Affect Different Groups
For Women
If your palpitations correlate with your menstrual cycle, track this carefully and share it with your doctor. Some women find that magnesium supplementation in the week before their period helps. During pregnancy, palpitations are extremely common and usually benign, but always mention them at prenatal visits. During menopause, discuss hormone replacement therapy (HRT) with your doctor if palpitations are severe, for some women, the benefits outweigh the risks.
For Athletes
Highly trained athletes often have lower resting heart rates (sometimes in the 40s), and their hearts adapt differently to stress. What might be abnormal for a sedentary person could be normal for you. However, new onset palpitations, especially during exercise, should never be ignored. Conditions like hypertrophic cardiomyopathy can be silent until they cause sudden problems during intense activity.
For Older Adults
As we age, the risk of significant arrhythmias like AFib increases substantially. After age 65, the prevalence jumps to about 9%, and it continues rising with each decade. Don’t dismiss new palpitations as “just getting older”, they deserve evaluation. The good news is that we have excellent treatments for most age-related arrhythmias.
For People with Anxiety Disorders
This creates a challenging cycle: anxiety causes palpitations, which cause anxiety about your heart, which causes more palpitations. Breaking this cycle often requires addressing both the physical and psychological components simultaneously. Work with both a cardiologist (to rule out heart issues and provide reassurance) and a mental health professional (to treat the underlying anxiety). Cognitive behavioral therapy has proven particularly effective for this scenario.
For People with Existing Heart Disease
If you’ve had a previous heart attack, have heart failure, or have known structural heart disease, palpitations need more aggressive evaluation. You’re at higher risk for dangerous arrhythmias, and what might be benign in someone else could be significant in your case. Don’t wait, contact your cardiologist promptly.
Myths and Misconceptions: Let’s Clear These Up
Myth #1: “Palpitations always mean something is seriously wrong with my heart.”
Reality: The vast majority of palpitations are benign. Studies show that even when thoroughly investigated, most palpitations in people without other cardiac symptoms or risk factors don’t indicate structural heart disease or dangerous arrhythmias.
Myth #2: “If my ECG is normal, I definitely don’t have a heart problem.”
Reality: A normal ECG is reassuring, but it only captures 10 seconds of your heart’s activity. Intermittent arrhythmias can be completely absent during that brief window. This is why ambulatory monitoring is sometimes needed.
Myth #3: “I’m too young to have heart problems.”
Reality: While many serious heart conditions are more common with age, arrhythmias can occur at any age. Some conditions, like SVT or certain congenital issues, often first appear in young adults. Age alone shouldn’t prevent appropriate evaluation.
Myth #4: “If stress is causing my palpitations, that means they’re all in my head.”
Reality: Stress-induced palpitations are real, physical events. The adrenaline your body releases in response to stress genuinely affects your heart’s electrical system. “Psychological” doesn’t mean “imaginary”, it means the trigger is stress rather than structural heart disease, but the palpitations themselves are very real.
Myth #5: “I should avoid all exercise if I have palpitations.”
Reality: Once serious causes are ruled out, regular exercise usually helps reduce palpitations over time by improving cardiovascular fitness and reducing baseline stress. The key is appropriate intensity and gradual progression. Discuss your specific situation with your doctor.
Myth #6: “Skipping beats means my heart is stopping.”
Reality: What feels like a “skipped beat” is usually a premature beat followed by a compensatory pause. Your heart doesn’t actually stop, it just beats out of turn, creating that flip-flop sensation. Occasional premature beats (PVCs or PACs) are extraordinarily common and usually harmless.
Questions to Ask Your Doctor
Going into a medical appointment prepared helps you get the most out of your time. Consider asking:
- Based on my symptoms and test results, what do you think is causing my palpitations?
- Are there any serious conditions we should rule out?
- What tests do you recommend, and why?
- Should I be restricting any activities while we figure this out?
- What symptoms should prompt me to go to the emergency room?
- Are there lifestyle changes you recommend specifically for my situation?
- If we don’t find a cause, what’s the next step?
- Should I see a cardiologist, or can you manage this in primary care?
- Could any of my current medications be contributing?
- What’s the likelihood this is something serious versus benign?
Don’t be afraid to ask for clarification if your doctor uses medical terminology you don’t understand. A good physician will explain things in plain language and ensure you understand the plan going forward.
Your Next Steps: Taking Action
Here’s a practical action plan based on your situation:
If your palpitations are occasional (less than once a week), brief (seconds to a few minutes), and not accompanied by warning signs:
- Start tracking them with a symptom diary
- Review and modify lifestyle factors (caffeine, alcohol, stress, sleep, hydration)
- Try vagal maneuvers when they occur
- Monitor for any changes in frequency or severity
- Schedule a routine checkup with your primary care doctor and mention the palpitations
If your palpitations are frequent (multiple times per week), prolonged, or bothersome enough to impact your life:
- Make an appointment with your doctor specifically to discuss them
- Bring your symptom diary with detailed observations
- Be prepared to discuss all medications, supplements, and lifestyle factors
- Ask about ambulatory monitoring if a basic ECG doesn’t capture episodes
If you experience any red flag symptoms:
- Don’t wait for a scheduled appointment
- Call your doctor immediately for same-day or next-day evaluation
- If symptoms are severe (chest pain, fainting, severe shortness of breath), go to the emergency room or call emergency services
If palpitations are triggering significant anxiety:
- Talk to your doctor about both the cardiac evaluation and mental health support
- Consider consulting with a therapist who specializes in health anxiety
- Explore mindfulness, meditation, or other stress-reduction techniques
- Join a support group for people experiencing palpitations
A Final Word of Reassurance
Living with palpitations can feel isolating and frightening. That sudden flutter in your chest can hijack your entire day, sending your mind spiraling into worst-case scenarios. But here’s what the medical evidence consistently shows: for the vast majority of people, palpitations are a nuisance, not a danger. They’re your heart’s way of responding to the complex interplay of stress, hormones, lifestyle factors, and the electrical system that keeps you alive.
At Hope Medical PC, we understand that heart concerns, whether they’re primarily physical, psychological, or a combination, deserve compassionate, thorough evaluation. Our team is here to help you understand what’s happening with your heart and guide you toward the peace of mind you deserve.
If you’d like to schedule an appointment to discuss your heart palpitations, contact us today. Your heart health is too important to leave to chance, and you don’t have to navigate this journey alone.
Additional Resources
For more information and support:
- American Heart Association: Comprehensive, evidence-based information on all aspects of heart health (www.heart.org)
- Mayo Clinic: Patient-friendly explanations of cardiac conditions and treatments (www.mayoclinic.org)
- Cleveland Clinic: Heart health resources and symptom checkers (www.clevelandclinic.org)
- Anxiety and Depression Association of America: Resources for managing health anxiety (www.adaa.org)
- National Alliance on Mental Illness: Support for mental health aspects of living with health concerns (www.nami.org)
Disclaimer: This article is for educational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read in this article. If you think you may have a medical emergency, call your doctor or emergency services immediately.