A heart cath can provide vital information about the health of your heart. It involves inserting a thin, flexible tube (catheter) into the heart’s arteries or chambers to visualize the blood vessels, measure pressures, and even take samples for analysis.
It helps physicians understand whether there are blockages in the arteries, how well the heart is pumping blood, and if there are any underlying structural problems, such as heart valve issues or congenital defects. Additionally, a heart cath is used to assess coronary artery disease (CAD), the leading cause of heart attacks.
In this guide, we’ll walk you through what happens during cardiac catheterisation, the potential risks, how long it takes, and what you can expect during recovery.
What Is Cardiac Catheterization?
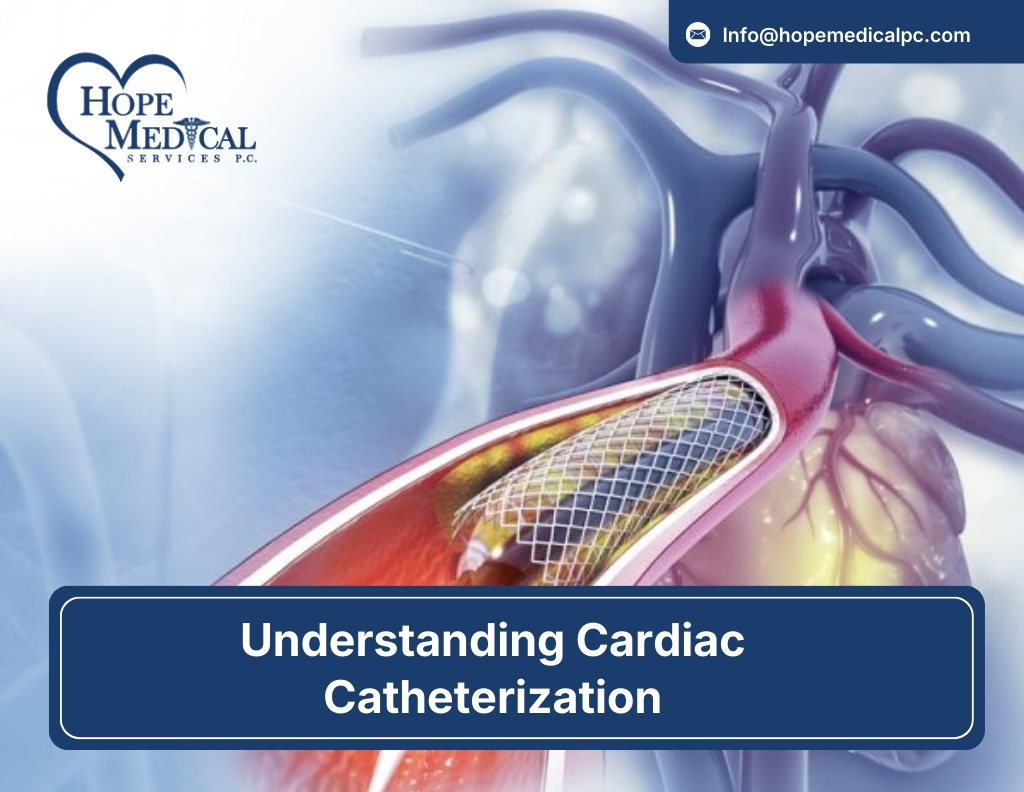
Cardiac catheterization, or heart cath, is a medical procedure used to diagnose and treat heart conditions. A thin, flexible tube called a catheter is inserted into a blood vessel in the groin, wrist, or arm and guided to the heart.
Using imaging technology, doctors can assess blood flow in the coronary arteries, check for blockages, measure pressures within the heart, and perform treatments like angioplasty or stent placement.
It is commonly used to diagnose coronary artery disease, evaluate heart function, and treat heart conditions such as blocked arteries. The procedure is minimally invasive and often provides vital information for guiding further treatment.
Step-by-Step Process of Cardiac Catheterization
Understanding what happens during a cardiac catheterisation procedure can help you feel more at ease and informed. Here’s a detailed look at what you can expect:
Before the Procedure
Before the procedure, your doctor will provide specific instructions. You may be asked to fast for several hours to ensure your stomach is empty during the procedure. You’ll also be given a sedative to help you relax, and a local anesthetic will be applied to the area where the catheter will be inserted, typically the groin or wrist.
The doctor will review your medical history and any medications you take. You may be instructed to stop taking certain medications, such as blood thinners, to reduce the risk of bleeding during the procedure.
An intravenous (IV) line will be inserted in your arm to provide fluids and medications during the procedure.
During the Procedure
Once you’re prepared, the procedure will begin. The process can take anywhere from 30 minutes to 2 hours, depending on the complexity of the case.
The doctor uses fluoroscopy (live X-ray) to guide the catheter into the coronary arteries and heart chambers. Contrast dye is injected through the catheter to highlight the arteries and help the physician detect any blockages or abnormalities.
If blockages or narrow arteries are found, the physician can perform additional treatments during the procedure, such as angioplasty (inflating a balloon to open blocked arteries) or inserting a stent to keep the artery open.
After the Procedure
Once the procedure is completed, the catheter will be removed, and pressure will be applied to the insertion site to stop any bleeding. You will be monitored for a short time, and you may be required to lie flat for a few hours to prevent any bleeding from the insertion site.
Most patients can go home the same day, although in some cases, you may need to stay in the hospital overnight for observation.
Follow-Up
Your doctor will schedule a follow-up appointment to discuss the results of the procedure and any further treatment that may be needed.
Risks and Complications of Cardiac Catheterization
Cardiac catheterization is a generally safe procedure with a high success rate. However, like any medical procedure, it’s not without its risks. Understanding these risks can help you feel more prepared and reduce any anxiety leading up to the procedure.
Imagine This:
You’ve just been told that a cardiac catheterization is the next step in diagnosing or treating your heart condition. You know it’s a routine procedure for many patients, but you might still wonder, “What could go wrong?”
Here’s what you need to know.
Bleeding or Hematoma at the Insertion Site:
After the catheter is inserted, there’s a chance of bleeding at the site, typically where the catheter entered your groin or wrist. Bruising or swelling is also possible. The doctors will apply pressure after the procedure to prevent this. While rare, if bleeding becomes severe, further medical intervention might be needed.
Infection:
In the case of a heart cath, the insertion site could become infected. However, doctors take extreme care to maintain a sterile environment, minimizing the chances of this happening. If an infection does occur, it’s usually treatable with antibiotics.
Heart Attack:
It’s hard to imagine that a heart cath could cause a heart attack. Yet, in rare cases, the procedure can inadvertently trigger a heart attack, especially if a blockage is found.
Stroke:
A blood clot can sometimes form during the procedure, which might travel to the brain. It’s one of the reasons doctors carefully monitor the heart and blood vessels throughout the entire procedure.
Arrhythmia:
Irregular heartbeats (arrhythmias) can sometimes occur when the catheter touches or stimulates the heart. Usually, these arrhythmias are temporary and manageable, but in some cases, they can be more severe, requiring additional treatment.
Damage to Blood Vessels or the Heart:
Though it’s extremely rare, the catheter could cause damage to blood vessels or even puncture the heart. This would require immediate treatment. However, advancements in catheter design and medical techniques have drastically reduced this risk.
How Often Do These Complications Occur?
The reality is that serious complications are very uncommon. Most patients undergo cardiac catheterization without any major issues. The success rate of the procedure is 95-98%, meaning that for the vast majority of people, the procedure goes smoothly.
However, each patient is unique, and certain factors can influence risk.
For example, those with diabetes, high blood pressure, or a history of heart disease may have slightly higher risks, which is why your doctor will closely review your medical history before scheduling the procedure.
How Long Does Cardiac Catheterization Take?
One of the most common questions patients have about cardiac catheterization is “How long will this take?” The duration of the procedure can vary depending on several factors, but here’s a general breakdown of what to expect.
1. Procedure Duration:
In most cases, the actual cardiac catheterization procedure will take between 30 minutes to 2 hours. This includes:
- Initial preparation: This part involves setting up the IV, applying local anesthesia, and prepping the catheter insertion site. It usually takes around 15–20 minutes.
- The procedure itself: Once everything is set, the catheter is inserted, and the doctor performs the diagnostic tests or interventions (such as angioplasty or stent placement). Depending on the complexity of the case, this could take anywhere from 30 minutes to 1.5 hours.
2. Factors Affecting Duration:
Several factors can influence how long the procedure takes, including:
- Complexity of the Case: If the doctor is simply performing a diagnostic angiogram to check for blockages, the procedure may be relatively quick. However, if the doctor needs to perform additional treatments (such as angioplasty, stenting, or biopsy), it will take longer.
- Number of Arteries Involved: If the doctor needs to check multiple arteries or perform a more detailed examination, the procedure may take longer.
- Patient-Specific Factors: Patients with complicated health histories or difficult-to-access blood vessels may require additional time.
3. Post-Procedure Recovery:
After the catheter is removed, patients are monitored for any immediate complications. You may need to stay in the hospital for several hours or overnight for observation. This is to ensure that you’re stable and there are no complications from the procedure.
- In the Recovery Room: You will be moved to a recovery area where medical staff will monitor your vital signs, and you may be asked to lie flat to prevent bleeding at the insertion site. This part of the process usually lasts about 1–3 hours.
- Discharge: If there are no complications, you might be able to go home the same day. For more complex cases or if you had interventions like stent placements, you might need to stay in the hospital for 1–2 days for further monitoring.
4. How Long Before You Feel Normal Again?
While the catheterisation procedure itself might take a few hours, the recovery process can take longer. Most people feel relatively normal after a few days but are advised to avoid strenuous activities or heavy lifting for a week or more.
Key Symptoms That Could Lead to a Heart Catheterisation
Cardiac catheterisation is often used to diagnose or treat heart conditions when certain symptoms or risk factors are present. But how do you know when it’s time to consider a heart cath? Here are some common symptoms and conditions that may lead to your doctor recommending the procedure.
Unexplained Chest Pain
Chest pain, also known as angina, is one of the most common reasons a doctor might recommend a cardiac catheterisation. If you’re experiencing chest pain that feels like pressure, tightness, or squeezing, and it doesn’t have an obvious cause (such as indigestion or a pulled muscle), it could be a sign of a blockage in the coronary arteries.
Shortness of Breath
If you suddenly find it difficult to catch your breath, especially during physical exertion, it might indicate that your heart is not pumping blood efficiently. This could be due to heart failure, blocked arteries, or damaged heart valves.
Dizziness or Fainting
Dizziness, lightheadedness, or fainting (syncope) can be a sign of a serious heart condition. These symptoms might be linked to abnormal heart rhythms (arrhythmias), which may require a cardiac catheterisation to investigate the cause.
History of Heart Disease or Risk Factors
If you have a family history of heart disease, or if you have any of the following risk factors, your doctor may recommend a heart cath even in the absence of obvious symptoms:
- High blood pressure (hypertension)
- High cholesterol levels
- Diabetes or prediabetes
- Smoking
- Sedentary lifestyle or obesity
- Older age (especially for men over 45 and women over 55)
- Family history of heart disease
If you have one or more of these risk factors, your doctor might recommend a heart catheterisation to assess the condition of your heart, even if you’re not experiencing specific symptoms.
Abnormal Results from Other Tests
Sometimes, a cardiac catheterisation is recommended after other diagnostic tests raise concerns. These tests may include:
- Stress Tests: If your stress test shows abnormal results, indicating reduced blood flow to the heart, a heart cath may be necessary to confirm the diagnosis.
- Echocardiogram: An ultrasound of the heart can reveal problems with the heart valves, heart chambers, or overall function. If there’s concern about a blockage or abnormality, a heart cath can provide a more detailed view.
- CT Scans or MRIs: These imaging techniques may show the presence of coronary artery disease or structural heart issues, leading to a recommendation for a heart cath.
Recovery and Aftercare Following Cardiac Catheterisation
After your cardiac catheterization, proper aftercare is essential for a smooth recovery. Most patients can go home the same day or after a short stay. Here’s what to expect during your recovery:
Immediate Post-Procedure Care
Once the procedure is complete, you’ll be monitored for several hours in the recovery area. Medical staff will keep an eye on your vital signs and the insertion site for any complications such as bleeding or swelling. You’ll need to rest and may be asked to lie flat for a few hours if the catheter was inserted through your groin.
At-Home Care
Limit physical activity for the first 24-48 hours. Avoid heavy lifting and strenuous activities for a week. Watch for any unusual symptoms like excessive swelling, pain, or bleeding at the insertion site. Contact your doctor if these occur. Drink plenty of fluids to help flush out the contrast dye used during the procedure.
Returning to Normal Activities
Most patients can return to normal activities within 1-2 weeks. Your doctor will give you specific instructions on when it’s safe to resume exercise or other physical activities. Follow-up appointments will be scheduled to ensure everything is healing as expected.
Long-Term Care
If you underwent a stent placement or other interventions, your doctor may prescribe medications to prevent blood clots and control blood pressure. A heart-healthy lifestyle, including regular exercise, a balanced diet, and quitting smoking, is crucial for long-term heart health.
Conclusion
While the procedure itself is relatively safe, it’s important to be aware of the potential risks and complications, as well as what to expect during recovery. With proper care and attention to aftercare instructions, most patients recover well and can return to their normal lives within a short period of time.
If you’ve been experiencing symptoms or have concerns about your heart, don’t wait. Schedule a Diagnostic Evaluation with our team of expert cardiologists today. Early detection and intervention can make all the difference in maintaining your heart health.